5 Triggers of Neuropathy and How to Get Relief
Neuropathy flare-ups can be triggered by factors like poor blood sugar control, stress, physical inactivity, and cold temperatures. To get relief, manage blood sugar, stay active, reduce stress, and avoid alcohol. A healthy diet and medications may also help reduce symptoms and improve circulation. At Northstar Joint and Spine, Board Certified Dr. Robert J. Nocerini, MD, offers professional care to help manage and alleviate neuropathy symptoms effectively. For more information, contact us today or schedule an appointment online. We are conveniently located at 7704 San Jacinto Pl Suite #200 Plano, TX 75024.
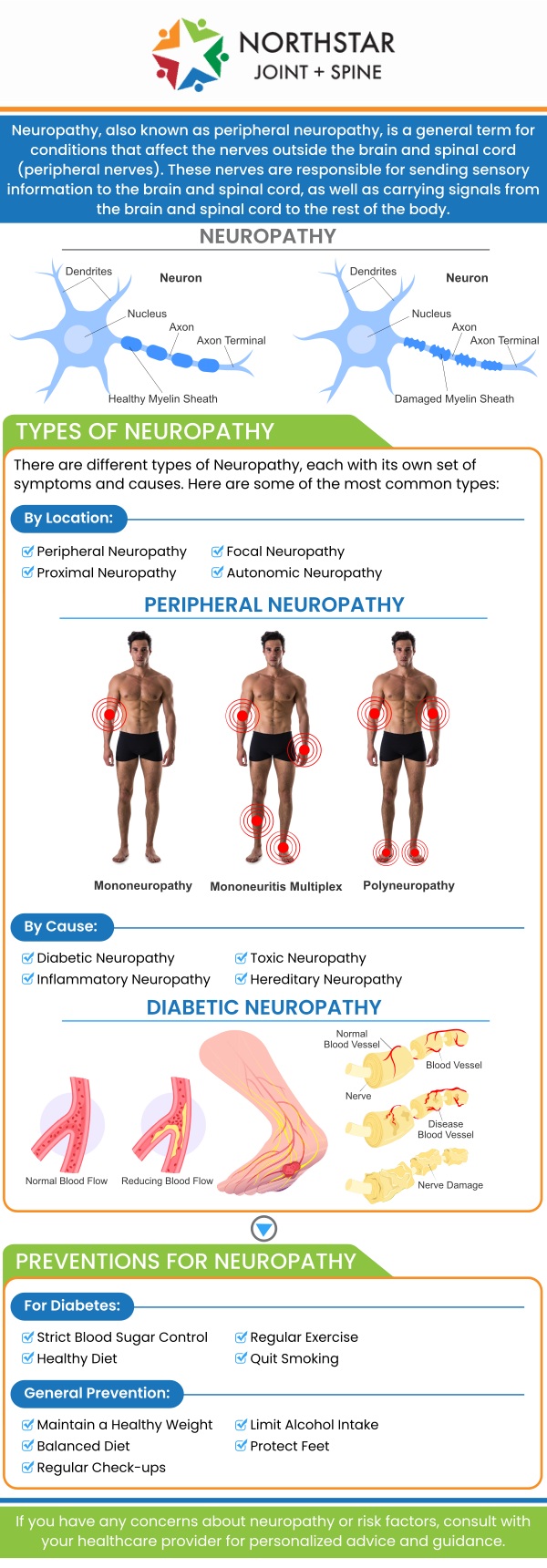
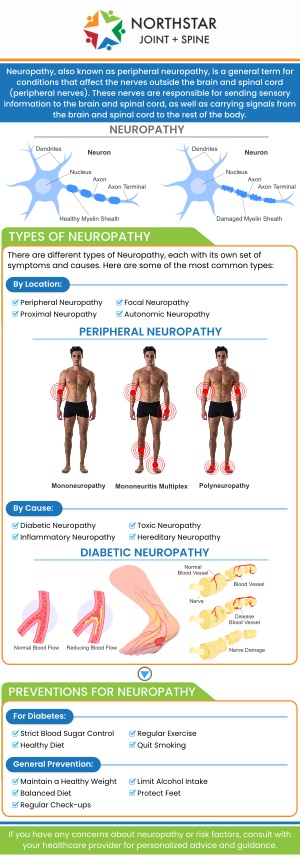
Table of Contents:
What are the most common triggers that worsen neuropathy symptoms?
How can identifying neuropathy triggers help in managing pain effectively?
Are there lifestyle factors that act as triggers for neuropathy flare-ups?
How can a doctor help manage neuropathy symptoms?
Triggers of Neuropathy and How to Get Relief with Board-Certified Dr. Robert J. Nocerini, MD at Northstar Joint and Spine
Neuropathy symptoms, such as pain, tingling, and numbness, can be worsened by several common triggers. Identifying these triggers is essential to managing and alleviating discomfort.
One of the most significant factors is poor blood sugar control in individuals with diabetes. Elevated blood sugar levels can cause damage to the nerves, intensifying neuropathy symptoms. Maintaining balanced blood glucose levels is crucial for managing neuropathy in diabetic patients.
Cold temperatures can also exacerbate neuropathy. When exposed to cold, blood vessels constrict, reducing circulation to the extremities. This can increase discomfort, numbness, and pain. Ensuring warmth in cooler environments can help alleviate these effects.
A lack of physical activity is another common trigger. Inactivity can lead to poor circulation and muscle weakness, which can worsen neuropathy. Regular movement helps improve blood flow and strengthen muscles, providing relief from symptoms.
Stress and anxiety can also heighten neuropathy symptoms. When under stress, the body releases hormones like cortisol, which can increase inflammation and sensitivity, leading to intensified discomfort.
Additionally, alcohol consumption can aggravate neuropathy symptoms, particularly in those with alcohol-related nerve damage. Alcohol can increase nerve sensitivity and interfere with nerve function.
Finally, certain medications may also contribute to worsening neuropathy symptoms. It is important for individuals to discuss their medications with a healthcare provider to avoid potential side effects.
Identifying neuropathy triggers plays a crucial role in effectively managing pain and improving overall quality of life. By understanding what worsens symptoms, individuals can take proactive steps to avoid or minimize these triggers, leading to better pain control.
For instance, recognizing that poor blood sugar control is a trigger in diabetic neuropathy allows individuals to focus on maintaining stable blood glucose levels through diet, exercise, and medication. This helps prevent further nerve damage and reduces discomfort.
Similarly, understanding the impact of cold temperatures on nerve pain can encourage people to dress warmly or avoid cold environments, minimizing pain flare-ups. Regular physical activity is another key element—by identifying inactivity as a trigger, individuals can incorporate movement into their daily routine to promote circulation and reduce muscle weakness, both of which can alleviate symptoms.
Managing stress is equally important. Recognizing that stress and anxiety can intensify neuropathy pain helps individuals adopt stress-reduction techniques, such as meditation or breathing exercises, to minimize their effect on nerve health.
Lastly, being aware of the role of medications or alcohol in worsening neuropathy symptoms allows individuals to make informed decisions with the guidance of their healthcare provider, ultimately leading to more effective pain management.
Several lifestyle factors can act as triggers for neuropathy flare-ups. Managing these factors is essential for controlling symptoms and reducing discomfort.
One significant factor is poor diet, particularly diets high in processed foods and sugars. Unhealthy eating habits can lead to elevated blood sugar levels, especially in individuals with diabetes, which can worsen neuropathy symptoms. A balanced diet rich in nutrients, including antioxidants and vitamins, can help protect nerve health and manage symptoms.
Lack of physical activity is another key contributor. Sedentary behavior can lead to poor circulation, muscle weakness, and increased nerve sensitivity, which can exacerbate neuropathy. Regular exercise, such as walking or swimming, promotes blood flow and strengthens muscles, helping to alleviate symptoms and improve mobility.
Excessive alcohol consumption can also trigger neuropathy flare-ups. Alcohol has neurotoxic effects and can worsen nerve damage, especially in individuals with alcohol-related nerve issues. Reducing or eliminating alcohol intake can prevent additional nerve damage and reduce pain.
Additionally, stress can worsen neuropathy symptoms by increasing inflammation and sensitivity in the body. Managing stress through relaxation techniques like meditation or deep breathing can help minimize its impact on nerve health.
Addressing these lifestyle factors can significantly improve neuropathy management and overall well-being.
A doctor can help manage neuropathy symptoms through a combination of diagnosis, treatment, and lifestyle recommendations tailored to the individual’s condition. The first step is an accurate diagnosis, where the doctor assesses the type of neuropathy, whether it’s related to diabetes, vitamin deficiencies, or another underlying condition. This allows for a targeted approach to managing symptoms.
Doctors may recommend medications to manage pain. For certain types of neuropathy, pain management strategies like nerve blocks or injections may be considered.
To address the root causes of neuropathy, doctors can guide blood sugar control for diabetic neuropathy, prescribe vitamin supplements for deficiencies, and recommend lifestyle changes like diet modifications to support nerve health. They may also suggest physical therapy to improve circulation, strengthen muscles, and reduce pain, especially for patients who experience difficulty moving.
Additionally, a doctor can advise on stress management techniques and relaxation exercises to reduce pain sensitivity, as stress is known to exacerbate symptoms. Regular monitoring and follow-up care ensure that treatments are effective and adjusted as needed, improving the patient’s overall quality of life.
At Northstar Joint and Spine, Board-Certified Dr. Robert Nocerini is dedicated to helping patients reduce pain and improve their quality of life through advanced neuropathy care. He understands that neuropathy can stem from several underlying causes, including diabetes, chronic inflammation, nutritional deficiencies, or nerve compression. Dr. Nocerini takes a comprehensive diagnostic approach to determine the root cause of each patient’s symptoms, using nerve studies and detailed evaluations to create a clear, personalized treatment path.
Dr. Nocerini’s care focuses on more than just symptom relief—he works to restore nerve health and function for long-term improvement. At Northstar Joint and Spine, Dr. Nocerini’s goal is to help patients regain comfort, mobility, and confidence, ensuring they can return to their daily activities with reduced pain and renewed vitality. For more information, contact us today or schedule an appointment online. We are conveniently located at 7704 San Jacinto Pl Suite #200 Plano, TX 75024. We serve patients from Plano TX, Willow Bend TX, Frisco TX, Allen TX, Addison TX, North Dallas TX, and surrounding areas.

Check Out Our 5 Star Reviews


Additional Services You May Need
▸ Back Pain
▸ Shoulder Pain
▸ Chronic Pain
▸ Epidural Steroid Injections
▸ Spinal Cord Stimulation
▸ Viscosupplementation
▸ Genicular Nerve Blocks
▸ Facet Injections
▸ Joint Injections
▸ Sacroiliac Joint Injections
▸ Lumbar and Cervical
▸ Facet Medial Branch Blocks
▸ Diagnostic Nerve Blocks
▸ Medication Management
▸ Neck Pain Doctor
▸ Diabetic Peripheral Neuropathy
▸ Headaches
▸ Suboxone
▸ Peripheral Nerve Stimulation
▸ Spine
▸ Joints
▸ Muscles
▸ Bones

Additional Services You May Need
▸ Back Pain
▸ Shoulder Pain
▸ Chronic Pain
▸ Epidural Steroid Injections
▸ Spinal Cord Stimulation
▸ Viscosupplementation
▸ Genicular Nerve Blocks
▸ Facet Injections
▸ Joint Injections
▸ Sacroiliac Joint Injections
▸ Lumbar and Cervical
▸ Facet Medial Branch Blocks
▸ Diagnostic Nerve Blocks
▸ Medication Management
▸ Neck Pain Doctor
▸ Diabetic Peripheral Neuropathy
▸ Headaches
▸ Suboxone
▸ Peripheral Nerve Stimulation
▸ Spine
▸ Joints
▸ Muscles
▸ Bones